Perhaps it is me becoming more demanding, but as the years have gone by, I have noticed that the general standard of medical student knowledge has been falling. At the risk of sounding like Grandpa Simpson ("Back in my day...") when I was a medical student I was so freaked out at everything that I was expected to learn and know that I'd constantly be looking things up (and forgetting them), and would always carry my trusty little Oxford Handbook of Clinical Medicine (or Surgery). Anything my registrar or consultant told me was gold, and I'd write it down. The more I listened to what they talked about the more I learned. This was particularly important given that I'm pretty bad with learning off the printed page. Anything I got asked that I didn't know the answer to was either an exercise in first principles (which have served me well) or a trip to the library.
Unfortunately, I have increasingly found that medical students (especially those doing PBL-type courses) have become less knowledgable, but more worryingly, less concerned about their lack of knowledge.
It is not uncommon that my students do not know how to test properly for visual acuity. They don't know what the normal intravascular volume of an average 60kg man is. They don't know what the inguinal ligament is, or what is at the mid-inguinal point. They don't know the difference between dysphasia and aphasia. They think that bunions and gouty tophi are the same thing as hallux valgus. Worst of all, they don't really seem to care.
I often walk into tutorials, planning on teaching a session on joint examination, or abdominal examination, CNS examination, or fluid-balance management, and end up getting no farther than explaining the difference between anterior / posterior, dorsal / ventral, superior / inferior, proximal / distal, or discussing the organs within the abdominal cavity, listing the cranial nerves and their functions, or discussing the waves of the JVP. This is basic knowledge missing from medical education today. There is so much focus on "validated educational processes", "problem based learning", "modular assessment and feedback" that it is making medical teaching inefficient. Students do not have enough application, time or ability to learn a large amount of knowledge in a few precious years. Instead, they learn a small amount of selected knowledge in an "educationally validated, continuously assessed" manner. We have forgotten that doctors (especially "junior" doctors) have always been relied upon to have a strong grasp of all aspects of medicine, and have all been seduced by the theoretical attractiveness of the PBL system.
These students can carry out the "moves" of a clinical examination. They ask the "right questions" on history taking. They have no concept, however, of why they are doing these things, or what the answers mean. The PBL course is supposed to encourage lateral thinking at the cost of basic sciences knowledge. I believe that it has failed in both regards when a final year medical student cannot tell that a patient has a false eye, or situs inversus, or is clinically dehydrated despite demonstrating numerous clinical sign that that is the case. When a patient with a weak, cool, numb leg automatically has "acute PVD" but a stroke is not a differential diagnosis. It is a disgrace when a final year medical student thinks that 20 seconds of scrubbing without removing their watch is acceptable before a surgical procedure. Even worse, they time their 20 seconds by singing 'Happy Birthday' in their heads. What is the world coming to?
I fear for our health system in the coming years. I fear even more, when I hear that postgraduate training will be shortened, rather than lengthened to compensate for these problems. We had better lower our expectations, because standards sure as hell will not be going up.
Friday, November 17, 2006
Wednesday, October 25, 2006
Stick me baby one more time
Unfortunately I have sustained my second needlestick injury in 12 months. This time, I was jabbed by one of my registrars. She managed to impale our scrub nurse as well in the same operation.
I cannot blame her for the event. We are new to each other, and still getting used to operating together. She is left-handed, and I am not. There is a clash on the operating table where we both like to put our hands. Goggles and visors reduce visibility but protect us from splashes. Double gloving reduces infection risk but reduces sensitivity in operating. Guarding the needle requires handling it an extra time with one's fingers.
Every protective manouevre we undertake compromises our ability to operate. If we are going to work with body fluids and sharp objects there will be a risk of exposure. We have to accept that fact of life, and draw an arbitrary line in the sand between our safety and our patients' wellbeing.
Those two blokes who got stuck in the mineshaft in Tasmania knew that they were at risk. What made that risk acceptable to them?
In any case, what irks me is not that it happened. Rather, it was the Infection Control Nurse* who came over with her forms and wanted to debrief us on all factors contributing to the needlestick injury. "What could we have done to avoid this event?" I could have said any number of things, like:
Even better was her parting comment. "Why should we risk our lives for our patients?" The fact is, every health worker risks their lives every day for all of their patients. I negotiate insane drivers to get to work every day. I risk being mugged walking from the car park to the hospital. I run the risk of being strangled by a delirious post-op patient every day. And I risk contracting an infectious disease every time I operate. I would love some way to eliminate all of these risks without inconveniencing me or my patients. Unfortunately, the only way this will happen is if I quit and stay home all day. I'm still considering that one.
*The Infection Control Nurse is a highly trained nurse practitioner / specialist clinical nurse consultant who has a plethora of duties, such as chastising people for needlestick injuries, chastising people for not washing their hands or using alcohol rubs, chastising people for standing in a room with a patient with "black colonies" (i.e. might have a remote chance of possibly having highly non-pathogenic VRE), and handing out jelly babies after torturing you with your annual influenza vaccination.
I cannot blame her for the event. We are new to each other, and still getting used to operating together. She is left-handed, and I am not. There is a clash on the operating table where we both like to put our hands. Goggles and visors reduce visibility but protect us from splashes. Double gloving reduces infection risk but reduces sensitivity in operating. Guarding the needle requires handling it an extra time with one's fingers.
Every protective manouevre we undertake compromises our ability to operate. If we are going to work with body fluids and sharp objects there will be a risk of exposure. We have to accept that fact of life, and draw an arbitrary line in the sand between our safety and our patients' wellbeing.
Those two blokes who got stuck in the mineshaft in Tasmania knew that they were at risk. What made that risk acceptable to them?
In any case, what irks me is not that it happened. Rather, it was the Infection Control Nurse* who came over with her forms and wanted to debrief us on all factors contributing to the needlestick injury. "What could we have done to avoid this event?" I could have said any number of things, like:
- not done the operation and let the patient suffer
- use blunt needles that would have botched the whole operation
- not worn visors, improved visibility and risk a splash injury
- refuse to work with left-handed female registrars
Even better was her parting comment. "Why should we risk our lives for our patients?" The fact is, every health worker risks their lives every day for all of their patients. I negotiate insane drivers to get to work every day. I risk being mugged walking from the car park to the hospital. I run the risk of being strangled by a delirious post-op patient every day. And I risk contracting an infectious disease every time I operate. I would love some way to eliminate all of these risks without inconveniencing me or my patients. Unfortunately, the only way this will happen is if I quit and stay home all day. I'm still considering that one.
*The Infection Control Nurse is a highly trained nurse practitioner / specialist clinical nurse consultant who has a plethora of duties, such as chastising people for needlestick injuries, chastising people for not washing their hands or using alcohol rubs, chastising people for standing in a room with a patient with "black colonies" (i.e. might have a remote chance of possibly having highly non-pathogenic VRE), and handing out jelly babies after torturing you with your annual influenza vaccination.
Saturday, October 14, 2006
Breaking Bad News
Yesterday I had the unfortunate task of informing a patient's family that he had passed away suddenly. He had died of (what I presume) was a ruptured abdominal aortic aneurysm (or AAA). This is where, over many years, the main artery carrying blood from the heart dilates and swells, getting weaker over time. In most people this is a very slow process, but for some people it can happen over a few short years, especially if they have high blood pressure, high cholesterol, and smoke. It can continue to dilate like a balloon until it bursts, at which point the patient has a 1 in 2 chance of making it to hospital alive, and a 1 in 4 chance of surviving surgery. Most patients have no idea that they have this problem, especially if they rarely see a doctor.
In any case, my patient had been previously well, but suddenly complained of back pain, collapsed, and had a cardiac arrest at home (a bad sign). He was transported to hospital by an ambulance crew and his rhythm restored, but things were not good. By the time he reached the operating theatre he had died and his belly was so full of blood it looked like a giant watermelon. All of this happened over the course of 2 hours, and there was hardly any time for the family to understand what was happening.
It is tragic enough breaking bad news to anybody, whether it be cancer or any other serious illness, the need to perform any operation to save life or limb, or a death. It is even worse when there is no time or opportunity for the patient or family members to realise that bad news might be coming.
Sadly I have to do this on a regular basis, and perhaps I have not learnt how to do it with grace, but rarely is there a meeting where at least one family member is not crying or asking "How could this have happened?". I have come to accept that no matter how empathic or caring I am, it is always distressing. I have learnt to carry on with my job after breaking the news (there is always paperwork), but make sure that a nurse or somebody else remains with the family to talk things over further and make sure nobody passes out.
So, my (limited) tips for breaking bad news:
In any case, my patient had been previously well, but suddenly complained of back pain, collapsed, and had a cardiac arrest at home (a bad sign). He was transported to hospital by an ambulance crew and his rhythm restored, but things were not good. By the time he reached the operating theatre he had died and his belly was so full of blood it looked like a giant watermelon. All of this happened over the course of 2 hours, and there was hardly any time for the family to understand what was happening.
It is tragic enough breaking bad news to anybody, whether it be cancer or any other serious illness, the need to perform any operation to save life or limb, or a death. It is even worse when there is no time or opportunity for the patient or family members to realise that bad news might be coming.
Sadly I have to do this on a regular basis, and perhaps I have not learnt how to do it with grace, but rarely is there a meeting where at least one family member is not crying or asking "How could this have happened?". I have come to accept that no matter how empathic or caring I am, it is always distressing. I have learnt to carry on with my job after breaking the news (there is always paperwork), but make sure that a nurse or somebody else remains with the family to talk things over further and make sure nobody passes out.
So, my (limited) tips for breaking bad news:
- Always sit down. Do this whether you are breaking bad news or not. It is a good habit for you, and encourages the family member to sit down. It also avoids many fainting episodes.
- Introduce yourself, then ask the family what they know. This lets the family talk first so you can get a gauge to how they will respond. Often they know what you are going to say.
- Get to the point. Family members know when you are beating about the bush, and it only gets worse if you put it off. That doesn't mean make it the first thing you say, just be tactful.
- Always have tissues handy. Nobody ever says no to tissues.
- Maintain eye contact until you have finished what you are saying. Staring at the wall or floor are bad no matter who you are talking to. It makes you look insincere.
- Don't try to say too much. They will not remember. It is silly to blabber on while people are crying. Blah blah blah, blah blah blah blah ...
- Don't get drawn into discussions about "What if?". Theories are theories, and given the selective memory of family members in grief, your conjectures may come back to haunt you. Usually in the Coroner's Court. This is especially true if you have strong opinions about what happened. You are probably upset too (and sometimes wrong).
- Always check if they have any questions, and offer to discuss and explain what happened at a later stage if they wish. This avoids many complaints.
- Tell them what will happen next. They do not want to make difficult decisions straight away, but they will want to know if the Coroner or Police will be involved, if an autopsy will be requested, when the body will be removed and to where.
- If they wish to see the body warn them of what they will see, especially if there are any tubes, wounds or deformities.
- Always make sure that somebody else is there with you to make sure you are not talking gibberish.
Tuesday, September 26, 2006
BB's Darker Days
Barbados Butterfly has just finished a series of posts entitled "The Darker Days" which are revealing yet insightful posts as always. Like any other profession, medicine is full of unsavoury experiences, often exacerbated by the expectations and pressures that society places upon doctors and nurses.
Working hours are often excessive, and there is no doubt that ridiculous >24 hour waking shifts should be outlawed, as well as on-call shifts where it is fully expected you will be kept awake.
I worry, however, about the needle swinging too far in the opposite direction... the doctor who in 5 years time struggles to find 38 hours of work to do each week. Last week I met some second-year paramedics, and some ICU nurses. I realised that my hourly pay is less than each of theirs, and the only thing that maintains gross income parity is the long hours I work. Imagine halving your income and doubling your training period because of the reduced patient exposure!
In her athlete analogy: "Sometimes their frequent injuries prevent them from reaching the heights they dreamed of, or force early retirement."
I must add that sometimes doctors do not realise that they do not have to reach the pinnacle of medical seniority in order to lead a full and productive professional life. There are a multitude of hidden and secret pathways into a long term medical career short of completing specialist and GP training. Unfortunately the options that are readily visible (e.g. career hospital HMO) are financially and professionally unrewarding in our current salary environment. I think it is inevitable this will change, though it has major implications for the structure of the Australian hospital system.
Working hours are often excessive, and there is no doubt that ridiculous >24 hour waking shifts should be outlawed, as well as on-call shifts where it is fully expected you will be kept awake.
I worry, however, about the needle swinging too far in the opposite direction... the doctor who in 5 years time struggles to find 38 hours of work to do each week. Last week I met some second-year paramedics, and some ICU nurses. I realised that my hourly pay is less than each of theirs, and the only thing that maintains gross income parity is the long hours I work. Imagine halving your income and doubling your training period because of the reduced patient exposure!
In her athlete analogy: "Sometimes their frequent injuries prevent them from reaching the heights they dreamed of, or force early retirement."
I must add that sometimes doctors do not realise that they do not have to reach the pinnacle of medical seniority in order to lead a full and productive professional life. There are a multitude of hidden and secret pathways into a long term medical career short of completing specialist and GP training. Unfortunately the options that are readily visible (e.g. career hospital HMO) are financially and professionally unrewarding in our current salary environment. I think it is inevitable this will change, though it has major implications for the structure of the Australian hospital system.
Wednesday, September 20, 2006
Are Doctors Society's Dinosaurs?
Tanveer Ahmed from Sydney wrote in today's Age suggesting that changes in medical education have not kept pace with other changes in the wider community, and that it is "one of the last bastions of the Old World left in our economy and requires a genuine shake-up... It is the East Germany of our society, waiting for its wall to fall."
Dr Ahmed (I don't know whether to refer to Tanveer as he or she) challenges the role of "systems, through colleges and apprentice-style training, that have effectively been unchanged for decades."
Let me tell you, Dr Ahmed, decades are not a long time. Our political system has not changed for over a century - is it time for a "radical shake-up"? Human anatomy has not been re-defined for at least several hundred years. Is it time to revamp the textbooks? Should we ditch the apprenticeship model that trains your plumber, electrician, painter or mechanic because it is not keeping pace with modern society?
There are a number of reasons that medical education and health systems have not been torn asunder and rebuilt every few years (despite what the ACCC may want).
Firstly, it is because small, incremental changes are happening all the time. This is how change is managed. Minor changes and improvements are introduced. They are assessed. If they work out they are kept, and if they don't they are reversed (let us hope the dilution of anatomy teaching will be reversed). We are not fighter pilots. We are doctors. The training produces flexible doctors who can make use of new technology, new information, new health system structures, and adapt to suit community requirements as they arise. If you knew that you needed fifteen left-handed dynamic hip-screw inserters in five years time you could train for that, but in five years time the DHS might be obsolete. And so will be your specialist DHS inserters.
Secondly, you may recall the Latin phrase "Primum non nocere" (First do no harm). Tearing down the public health system and medical education in one fell swoop would cause a lot of harm, long before it did any good, especially when no adequate replacement is conceived or planned for.
Thirdly, my favourite saying: "If it ain't broke, don't fix it". As you say, the current arrangement of "cheap labour in underfunded public hospitals... suits many people in authority, both within the profession and in government". Well, let me tell you, it also suits the common citizen holding their Medicare card, who gets first-world health-care for 1% of their gross taxable income each year. As doctors we may grumble and bitch about our lack of pay, long working hours, lack of recognition, long training periods, and no social life, but aren't you the least bit proud that you are providing the majority of your patients with health care that is the envy of many countries around the world?
If anything, the most frustrating part about being a doctor in Australia is that given state and federal funding constraints we can only provide some of the services to some of the people some of the time, but of what we do deliver it is still top quality care. Yes, my pay after 16 years of training is paltry compared to my younger cousin who reprograms the ATM system for a major bank, or my recently-graduated friend who advises semi-private health insurance companies how to waste the wads of cash they make every second. But I have the satisfaction of a patient coming up to me and saying "Thankyou for improving or saving my life" every now and again, and that makes me proud of what I do, despite the fact that the public health system uses and abuses me.
My concern is that if Tanveer's opinion translates to a general perception that doctors are over-trained, then we are looking at the inevitable extinction of the traditional doctor. No longer will we have a health professional who is expected to deal with anything and everything that could possibly come through the door, and to have a good grasp of all the other facets of health care and medicine that affect their patients - we will have a workflow-oriented, productivity-driven, multidisciplinary team-based system with cannulation technicians, specialist nurse practitioners, phlebotomists, reporting radiographers, analytic biochemistry technicians, and diagnostic hygiene specialists who will hold a committee meeting every half hour to discuss why the patient in Cubicle 21 is deviating from the ingrown toenail clinical pathway. There will not be a doctor to be seen because they will be unnecessary. Is this what the Productivity Commission wants?
I might as well retire today. Perhaps we should not be reforming our health-care system or medical training, just our expectations of what it should deliver.
Dr Ahmed (I don't know whether to refer to Tanveer as he or she) challenges the role of "systems, through colleges and apprentice-style training, that have effectively been unchanged for decades."
Let me tell you, Dr Ahmed, decades are not a long time. Our political system has not changed for over a century - is it time for a "radical shake-up"? Human anatomy has not been re-defined for at least several hundred years. Is it time to revamp the textbooks? Should we ditch the apprenticeship model that trains your plumber, electrician, painter or mechanic because it is not keeping pace with modern society?
There are a number of reasons that medical education and health systems have not been torn asunder and rebuilt every few years (despite what the ACCC may want).
Firstly, it is because small, incremental changes are happening all the time. This is how change is managed. Minor changes and improvements are introduced. They are assessed. If they work out they are kept, and if they don't they are reversed (let us hope the dilution of anatomy teaching will be reversed). We are not fighter pilots. We are doctors. The training produces flexible doctors who can make use of new technology, new information, new health system structures, and adapt to suit community requirements as they arise. If you knew that you needed fifteen left-handed dynamic hip-screw inserters in five years time you could train for that, but in five years time the DHS might be obsolete. And so will be your specialist DHS inserters.
Secondly, you may recall the Latin phrase "Primum non nocere" (First do no harm). Tearing down the public health system and medical education in one fell swoop would cause a lot of harm, long before it did any good, especially when no adequate replacement is conceived or planned for.
Thirdly, my favourite saying: "If it ain't broke, don't fix it". As you say, the current arrangement of "cheap labour in underfunded public hospitals... suits many people in authority, both within the profession and in government". Well, let me tell you, it also suits the common citizen holding their Medicare card, who gets first-world health-care for 1% of their gross taxable income each year. As doctors we may grumble and bitch about our lack of pay, long working hours, lack of recognition, long training periods, and no social life, but aren't you the least bit proud that you are providing the majority of your patients with health care that is the envy of many countries around the world?
If anything, the most frustrating part about being a doctor in Australia is that given state and federal funding constraints we can only provide some of the services to some of the people some of the time, but of what we do deliver it is still top quality care. Yes, my pay after 16 years of training is paltry compared to my younger cousin who reprograms the ATM system for a major bank, or my recently-graduated friend who advises semi-private health insurance companies how to waste the wads of cash they make every second. But I have the satisfaction of a patient coming up to me and saying "Thankyou for improving or saving my life" every now and again, and that makes me proud of what I do, despite the fact that the public health system uses and abuses me.
My concern is that if Tanveer's opinion translates to a general perception that doctors are over-trained, then we are looking at the inevitable extinction of the traditional doctor. No longer will we have a health professional who is expected to deal with anything and everything that could possibly come through the door, and to have a good grasp of all the other facets of health care and medicine that affect their patients - we will have a workflow-oriented, productivity-driven, multidisciplinary team-based system with cannulation technicians, specialist nurse practitioners, phlebotomists, reporting radiographers, analytic biochemistry technicians, and diagnostic hygiene specialists who will hold a committee meeting every half hour to discuss why the patient in Cubicle 21 is deviating from the ingrown toenail clinical pathway. There will not be a doctor to be seen because they will be unnecessary. Is this what the Productivity Commission wants?
I might as well retire today. Perhaps we should not be reforming our health-care system or medical training, just our expectations of what it should deliver.
Thursday, September 14, 2006
Doctor Death - or Doctors' Deaths
It was only a matter of time before the papers wrote it up (Young doctors succumb to killing pressures on the ward, The Age 13/9/06) but it concerns me as always that the focus is on working hours (Young doctors' rest-deprived life, The Age 14/9/06). I have written about this before (Doctors get stressed too).
Yes, as hospital doctors we work long hours. Yes, most hospitals have little incentive to reduce working hours (despite the AMA's Safe Hours campaign - potentially flawed as it may be). But don't confuse long working hours with causing doctor suicides. It is a single factor among many others, including long-term responsibilities for patient care; work conflicts with other medical teams and other staff; mixed loyalties to patients, bosses, friends, colleagues, and families.
Personally, I believe that many of these stressors are offset by the rewards: that satisfying feeling of successfully fixing a patient's problem, and talking to a grateful patient and family; being appropriately remunerated for one's services; having a sense of standing within the community; spending fruitful and rewarding time with one's friends and family. I work long hours. I experience stress at work. But I experience the rewards and I do not mind. Some of my colleagues, however, are denied those rewards on a regular basis.
Stressors will not go away. To take them away requires a massive restructuring of our health system which is economically impossible, and despite a lot of empty rhetoric from state and federal governments, is not in their interests. We may whine on about reducing working hours (at the cost of prolonging postgraduate medical training), employing more junior hospital doctors (Where will they come from? Where will they go afterwards? Where is the career path for "hospitalists"?), buying more fancy equipment (equipment is cheap, people are expensive), but at the end of the day, it is all political pseudospeak.
You want to know what the real factor in doctor suicides is? Take a group of motivated, intelligent, organised people. Give them access to lethal drugs and the knowledge of how to kill themselves quickly and painlessly. A small proportion (just like the general community) will develop suicidal ideations. A smaller proportion still will attempt suicide. Unlike the general population, however, every single doctor will succeed. There are no "attempted suicides" among doctors. No random pill-swallowing. No jumping off rooftops. No lying in front of trucks. If a doctor tries to commit suicide, he or she will succeed. Unless they don't really want to.
If you want to make doctors feel better, and discourage them from committing suicide in the first place, then we need to improve the general mental health of doctors. Reducing work stress is part of this, but personally I feel that we need to fix the eroding status that doctors have in our society. We are not commodities to be traded from country to country. We are not bargaining chips to be swapped between government consortia. Talking down our salaries means talking down our value to the community. Make hospital doctors feel wanted, and they will want to stay. Make hospital doctors feel valued, and they will want to live.
Yes, as hospital doctors we work long hours. Yes, most hospitals have little incentive to reduce working hours (despite the AMA's Safe Hours campaign - potentially flawed as it may be). But don't confuse long working hours with causing doctor suicides. It is a single factor among many others, including long-term responsibilities for patient care; work conflicts with other medical teams and other staff; mixed loyalties to patients, bosses, friends, colleagues, and families.
Personally, I believe that many of these stressors are offset by the rewards: that satisfying feeling of successfully fixing a patient's problem, and talking to a grateful patient and family; being appropriately remunerated for one's services; having a sense of standing within the community; spending fruitful and rewarding time with one's friends and family. I work long hours. I experience stress at work. But I experience the rewards and I do not mind. Some of my colleagues, however, are denied those rewards on a regular basis.
Stressors will not go away. To take them away requires a massive restructuring of our health system which is economically impossible, and despite a lot of empty rhetoric from state and federal governments, is not in their interests. We may whine on about reducing working hours (at the cost of prolonging postgraduate medical training), employing more junior hospital doctors (Where will they come from? Where will they go afterwards? Where is the career path for "hospitalists"?), buying more fancy equipment (equipment is cheap, people are expensive), but at the end of the day, it is all political pseudospeak.
You want to know what the real factor in doctor suicides is? Take a group of motivated, intelligent, organised people. Give them access to lethal drugs and the knowledge of how to kill themselves quickly and painlessly. A small proportion (just like the general community) will develop suicidal ideations. A smaller proportion still will attempt suicide. Unlike the general population, however, every single doctor will succeed. There are no "attempted suicides" among doctors. No random pill-swallowing. No jumping off rooftops. No lying in front of trucks. If a doctor tries to commit suicide, he or she will succeed. Unless they don't really want to.
If you want to make doctors feel better, and discourage them from committing suicide in the first place, then we need to improve the general mental health of doctors. Reducing work stress is part of this, but personally I feel that we need to fix the eroding status that doctors have in our society. We are not commodities to be traded from country to country. We are not bargaining chips to be swapped between government consortia. Talking down our salaries means talking down our value to the community. Make hospital doctors feel wanted, and they will want to stay. Make hospital doctors feel valued, and they will want to live.
Friday, June 23, 2006
Grand Rounds v2.38
Perhaps a little late, but Grand Rounds is up at The Haversian Canal - and The Paper Mask gets a mention too!
Wednesday, June 07, 2006
Can't you take a hint?
 Betty was 95. She lived in a nursing home. She was delirious and bedbound. She had diabetes, emphysema, untreatable ischaemic heart disease, and a recent stroke. And now she had a fever and a gangrenous leg.
Betty was 95. She lived in a nursing home. She was delirious and bedbound. She had diabetes, emphysema, untreatable ischaemic heart disease, and a recent stroke. And now she had a fever and a gangrenous leg.She was going to die, sooner or later.
"She's a fighter" her son said. "Before she became delirious, she told me that she'd rather lose her leg than die."
I didn't say what I was thinking - "This is not a life. You are just torturing her. She is going to die anyway."
Instead I say: "I appreciate what you are saying, but you must understand that amputating her leg has a very high chance of killing her, both immediately and in the near future. And even if she were to survive that operation her quality of life would only be worse, not better. She would definitely never walk again."
"We know that, doc, but we'd rather she die under an anaesthetic than like this. We know that's what she'd want. She doesn't walk as it is."
Perhaps I am weak, but I cannot flat out refuse to do it. I don't know for certain that she will die. She might pull through. Her chances are poor, but they are not zero.
Two days later she is awake and talking to her family. She thanks me for doing the amputation, and goes back to her nursing home. A week later I hear that she has had a "heart attack" and has passed away.
-----
Jerry is 70. He came from a hostel. He was confused but relatively independent , until he developed acute appendicitis. A diagnosis made at laparotomy. He makes a good recovery, but unfortunately, a pressure sore develops on his heel. Bone is exposed, and needs debridement. Malnutrition limits what healing is present. The arterial supply is limited. He is too confused to eat. He needs nasogastric feeding, an angiogram and a small operation to clean his ulcer."We don't think he would appreciate it, doc." said the daughter. "He doesn't know what is going on. He won't want to risk losing his leg. We're sure he wouldn't want a tube in his nose. Why can't we let him die with dignity?"
"He is not going to die anytime soon." I say. "But this ulcer will be with him for the rest of his days unless we remove the bone and put a skin graft on it. The ulcer won't kill him but it will cause him pain."
"We think he's had enough. We'd like to speak to the palliative care nurse."
Palliative care takes him over and he is dosed up to his eyeballs with subcut morphine. A month later he is still alive. I wonder how long he will last at the hospice, and how much morphine he can handle.
-----
 John was 65, living with cerebral palsy, schizophrenia, and a recently fractured humerus. Paraplegic and confused. He had recently been transferred into a nursing home where he was fully dependent. Now he had severe, sudden onset abdominal pain. There was gas under his diaphragm. There was no doubt he had a perforated viscus. Probably a duodenal ulcer. Laparotomy would be straightforward and life-saving. "I'm not going to die, doc. Just give me some pain killers and let me go home. I don't want an operation." he said.
John was 65, living with cerebral palsy, schizophrenia, and a recently fractured humerus. Paraplegic and confused. He had recently been transferred into a nursing home where he was fully dependent. Now he had severe, sudden onset abdominal pain. There was gas under his diaphragm. There was no doubt he had a perforated viscus. Probably a duodenal ulcer. Laparotomy would be straightforward and life-saving. "I'm not going to die, doc. Just give me some pain killers and let me go home. I don't want an operation." he said.There was no family. They had abandoned him years ago. His sister hung up the phone when rung at 2am in the morning. The GP that normally treated John was on holiday. From the little information I could gather, his quality of life was non-existent. Who do I ask? Who do I turn to? Do I have the right to decide whether to operate or palliate? In his incapacitated state does he have the right to refuse surgery?
So I passed the buck, and called the Chief Medical Officer. "What do I do?" I ask. "You are authorised under law to do as you see fit. As the clinician on duty, the hospital will support your decision." came the drab reply over the telephone.
So I wrote up the omeprazole, turned up the morphine infusion, and went back to sleep.
Tuesday, June 06, 2006
Happy Happy Joy Joy
Yesterday I received some very good news. A significant amount of time was spent celebrating, and a significant amount of time this morning was spent recovering. Luckily, the hangover had subsided by the time the emergency redo laparotomy rolled in the door at 1300h. Obviously bad news does not care when good news arrives.
Thursday, June 01, 2006
Time goes quickly when you're having fun
Dr Flea was recently concerned that down-under surgeons have too much time on their hands. I must point out otherwise. Just because clocks run backwards here (I'd say counter-clockwise, but if all clocks ran counter-clockwise, then does that mean than clocks that run clockwise are running backwards and not forwards?) does not mean that they run any slower, or faster, or... you know what I mean.
The only exception is once a day when we are approximately one-Earth's diameter closer to the sun, because the sun's gravitational field is infinitesimally stronger and therefore time does in fact slow down compared to the other side of the world. Though we probably make up for it about 12 hours later. Or sooner. Whatever.
The point is that I have been very, very busy, and will hopefully have more time on my hands soon to work on my Probability of Malpractice Suit Monitor. The problem at the moment is the incessant beeping. I must recalibrate it... it never seems to fall below 5%.
The only exception is once a day when we are approximately one-Earth's diameter closer to the sun, because the sun's gravitational field is infinitesimally stronger and therefore time does in fact slow down compared to the other side of the world. Though we probably make up for it about 12 hours later. Or sooner. Whatever.
The point is that I have been very, very busy, and will hopefully have more time on my hands soon to work on my Probability of Malpractice Suit Monitor. The problem at the moment is the incessant beeping. I must recalibrate it... it never seems to fall below 5%.
Thursday, May 25, 2006
Doctors Behaving Badly
This time it is medical students, not doctors.
What is wrong with you people? Can't you guys just leave Paris Hilton alone?
Surely you have better things to do. As for me, I'm relieving stress with my hobby of Bonsai Kittens (mirror available here).
"Med students expelled for secret sex tape"
Last Update: Thursday, May 25, 2006. 7:02pm (AEST)
Four students have been expelled for posting a secret sex tape on a campus website at the James Cook University in north Queensland.
It is alleged four men, including three medical students, secretly taped the woman in a sexual act and posted a link to the video on a college intranet website.
One of the men is believed to the woman's ex-boyfriend.
The university says its investigation found the men behaved inappropriately and it has cancelled their enrolments.
One of the men will be eligible to return to the campus in 2008.
The others will not be allowed to return until 2009.
The university says it cannot comment further at this stage as the men may appeal against the decision.
What is wrong with you people? Can't you guys just leave Paris Hilton alone?
Surely you have better things to do. As for me, I'm relieving stress with my hobby of Bonsai Kittens (mirror available here).
Friday, May 19, 2006
Absence noted
Apologies for the recent lack of activity. I can assure readers that there are very good reasons for this, and, no, I do not care to share them at this time. If all goes well, I shall explain in due course, though probably after a lengthy delay.
On other topics, I completed the AMA Safe Hours Survey at the start of the week. I did not score well. -37 on the impairment scale. I can tell you, that I feel every point of that scale. 4 hours sleep over 48 hours is not healthy.
I would encourage all Australian doctors to complete the survey. If nothing else, it will demonstrate whether I am a statistical anomaly or not.
On other topics, I completed the AMA Safe Hours Survey at the start of the week. I did not score well. -37 on the impairment scale. I can tell you, that I feel every point of that scale. 4 hours sleep over 48 hours is not healthy.
I would encourage all Australian doctors to complete the survey. If nothing else, it will demonstrate whether I am a statistical anomaly or not.
Wednesday, May 10, 2006
Grand Rounds v2.33
Grand Rounds is up at Aetiology. I'm amazed how many medical blogs are out there. I'm even more amazed that people have time to read them all and summarise them as Grand Rounds.
Tara at Aetiology calls me weird in this week's Grand Rounds. I have no idea why.
Tara at Aetiology calls me weird in this week's Grand Rounds. I have no idea why.
Monday, May 08, 2006
The pS monitor
Psst, don't tell anyone, but I am working on a secret new medical device - the pS monitor. Let me explain - imagine me as a young Trauma Surgery registrar, trembling with a combination of fear and cold (why are hospitals so cold at night?) as I get called to my first trauma in the middle of the night.
"65 year old man, previously well. Single vehicle MCA, ejected through windscreen. 4-wheel drive versus tree in an 80 k zone." As the ambulance paramedic continues talking, an extra ED nurse starts filling in her clipboard. "Patient was unconscious at the scene with GCS 5 (tick) BP 90/60 (tick) Resp Rate 20 (tick), he was diaphoretic and shut down. Intubated at the scene with difficulty."
"Why say 'diaphoretic' when you can say 'sweaty'?" I think to myself. It annoys me as much as when people say 'pussy' instead of 'purulent'. I have dreams of infected abscesses exuding cats. Call me weird if you will.
As the ambo keeps talking, I start examining the patient. He is intubated, unconscious and paralysed. I can hear breath sounds throughout the lungfields and there's no dullness on percussion. There are some clinically fractured ribs on the right. "Good," I think, "No need for a chest tube here - yet." BP 100/60, Pulse rate 100, thankfully the fluids are going in through two nice big 16G IVs.
 Primary survey over, I complete my secondary survey - forehead laceration with a small right occipital haematoma, cervical spine roughly in place (and patient asleep), clavicles and upper limbs intact, rib crepitus on the right, lax, paralysed abdomen, pelvis intact, and a left femoral shaft fracture. As I describe my findings for the benefit of our ED registrar, I see the nurse in the corner of my eye going "tick, tick, tick-tick". She seems strangely quiet as I check his urethra and do a PR. I'm much happier when I feel bounding pedal pulses. Chest and Cervical Spine X-rays show some early pulmonary contusion, no haemo- or pneumothorax and aforementioned rib fractures.
Primary survey over, I complete my secondary survey - forehead laceration with a small right occipital haematoma, cervical spine roughly in place (and patient asleep), clavicles and upper limbs intact, rib crepitus on the right, lax, paralysed abdomen, pelvis intact, and a left femoral shaft fracture. As I describe my findings for the benefit of our ED registrar, I see the nurse in the corner of my eye going "tick, tick, tick-tick". She seems strangely quiet as I check his urethra and do a PR. I'm much happier when I feel bounding pedal pulses. Chest and Cervical Spine X-rays show some early pulmonary contusion, no haemo- or pneumothorax and aforementioned rib fractures.
 The left leg goes into traction, and then off for a CT scan of his head (left parietal contre-coup contusion with a small subdural haematoma - "tick-tick"), neck (normal - but the collar stays on), and abdomen (minor hepatic laceration - "tick"). The femur gets nailed while the neurosurgeons put in an ICP monitor and the patient goes to ICU intubated with a Philadelphia collar until he wakes up.
The left leg goes into traction, and then off for a CT scan of his head (left parietal contre-coup contusion with a small subdural haematoma - "tick-tick"), neck (normal - but the collar stays on), and abdomen (minor hepatic laceration - "tick"). The femur gets nailed while the neurosurgeons put in an ICP monitor and the patient goes to ICU intubated with a Philadelphia collar until he wakes up.
I'm left wondering what all that ticking is about - and then I realise... it is the scoring for the trauma audit. Our nurse is calculating the patient's probability of survival. And for my patient it is 27.6%. Do I care what it was? Would I have stopped, had I known his poor likelihood of survival? I don't think so. But it looks like a great business opportunity to me.
 That's why I am introducing the digital Probablility of Survival (pS) monitor. This little device will use advanced voice-recognition software as the registrar describes his findings, and with some fancy wireless networking, will pick up the observations from all other monitoring equipment. Using my secret modified algorithm a much more accurate probability of survival will be calculated every 5 seconds, so that you can know exactly when to stop resuscitation.
That's why I am introducing the digital Probablility of Survival (pS) monitor. This little device will use advanced voice-recognition software as the registrar describes his findings, and with some fancy wireless networking, will pick up the observations from all other monitoring equipment. Using my secret modified algorithm a much more accurate probability of survival will be calculated every 5 seconds, so that you can know exactly when to stop resuscitation.
Imagine all the unnecessary exploratory laparotomies and ICU time that could be avoided. All the CTs and MRIs and IVC filters that wouldn't be wasted. We could resuscitate people until their pS fell below the economically viable threshold for the hospital. I don't believe in the device one little bit, but at US$1000 each, 5 for each ED worldwide, imagine the money I'd make!
I can't wait until my next invention is ready... the B-S monitor.
"65 year old man, previously well. Single vehicle MCA, ejected through windscreen. 4-wheel drive versus tree in an 80 k zone." As the ambulance paramedic continues talking, an extra ED nurse starts filling in her clipboard. "Patient was unconscious at the scene with GCS 5 (tick) BP 90/60 (tick) Resp Rate 20 (tick), he was diaphoretic and shut down. Intubated at the scene with difficulty."
"Why say 'diaphoretic' when you can say 'sweaty'?" I think to myself. It annoys me as much as when people say 'pussy' instead of 'purulent'. I have dreams of infected abscesses exuding cats. Call me weird if you will.
As the ambo keeps talking, I start examining the patient. He is intubated, unconscious and paralysed. I can hear breath sounds throughout the lungfields and there's no dullness on percussion. There are some clinically fractured ribs on the right. "Good," I think, "No need for a chest tube here - yet." BP 100/60, Pulse rate 100, thankfully the fluids are going in through two nice big 16G IVs.
 Primary survey over, I complete my secondary survey - forehead laceration with a small right occipital haematoma, cervical spine roughly in place (and patient asleep), clavicles and upper limbs intact, rib crepitus on the right, lax, paralysed abdomen, pelvis intact, and a left femoral shaft fracture. As I describe my findings for the benefit of our ED registrar, I see the nurse in the corner of my eye going "tick, tick, tick-tick". She seems strangely quiet as I check his urethra and do a PR. I'm much happier when I feel bounding pedal pulses. Chest and Cervical Spine X-rays show some early pulmonary contusion, no haemo- or pneumothorax and aforementioned rib fractures.
Primary survey over, I complete my secondary survey - forehead laceration with a small right occipital haematoma, cervical spine roughly in place (and patient asleep), clavicles and upper limbs intact, rib crepitus on the right, lax, paralysed abdomen, pelvis intact, and a left femoral shaft fracture. As I describe my findings for the benefit of our ED registrar, I see the nurse in the corner of my eye going "tick, tick, tick-tick". She seems strangely quiet as I check his urethra and do a PR. I'm much happier when I feel bounding pedal pulses. Chest and Cervical Spine X-rays show some early pulmonary contusion, no haemo- or pneumothorax and aforementioned rib fractures. The left leg goes into traction, and then off for a CT scan of his head (left parietal contre-coup contusion with a small subdural haematoma - "tick-tick"), neck (normal - but the collar stays on), and abdomen (minor hepatic laceration - "tick"). The femur gets nailed while the neurosurgeons put in an ICP monitor and the patient goes to ICU intubated with a Philadelphia collar until he wakes up.
The left leg goes into traction, and then off for a CT scan of his head (left parietal contre-coup contusion with a small subdural haematoma - "tick-tick"), neck (normal - but the collar stays on), and abdomen (minor hepatic laceration - "tick"). The femur gets nailed while the neurosurgeons put in an ICP monitor and the patient goes to ICU intubated with a Philadelphia collar until he wakes up.I'm left wondering what all that ticking is about - and then I realise... it is the scoring for the trauma audit. Our nurse is calculating the patient's probability of survival. And for my patient it is 27.6%. Do I care what it was? Would I have stopped, had I known his poor likelihood of survival? I don't think so. But it looks like a great business opportunity to me.
 That's why I am introducing the digital Probablility of Survival (pS) monitor. This little device will use advanced voice-recognition software as the registrar describes his findings, and with some fancy wireless networking, will pick up the observations from all other monitoring equipment. Using my secret modified algorithm a much more accurate probability of survival will be calculated every 5 seconds, so that you can know exactly when to stop resuscitation.
That's why I am introducing the digital Probablility of Survival (pS) monitor. This little device will use advanced voice-recognition software as the registrar describes his findings, and with some fancy wireless networking, will pick up the observations from all other monitoring equipment. Using my secret modified algorithm a much more accurate probability of survival will be calculated every 5 seconds, so that you can know exactly when to stop resuscitation.Imagine all the unnecessary exploratory laparotomies and ICU time that could be avoided. All the CTs and MRIs and IVC filters that wouldn't be wasted. We could resuscitate people until their pS fell below the economically viable threshold for the hospital. I don't believe in the device one little bit, but at US$1000 each, 5 for each ED worldwide, imagine the money I'd make!
I can't wait until my next invention is ready... the B-S monitor.
Saturday, April 29, 2006
Sister, I'm Speechless.
 I don't know what to say. While surfing, I noticed Kim from Emergiblog's support for the concept of a US National Nurse via a US Congress Bill HR903. I can only presume this is a nursing equivalent of the US Surgeon-General.
I don't know what to say. While surfing, I noticed Kim from Emergiblog's support for the concept of a US National Nurse via a US Congress Bill HR903. I can only presume this is a nursing equivalent of the US Surgeon-General.Now, I had always thought it a bit odd that the US had a Surgeon-General, but fair enough, that's what they decided on. His or her job is to go around promoting public health. That's great. In fact, the Surgeon-General's specific duties are:
- To administer the U.S. Public Health Service (PHS) Commissioned Corps, which is a uniquely expert, diverse, flexible, and committed career force of public health professionals who can respond to both current and long-term health needs of the Nation;
- To provide leadership and management oversight for PHS Commissioned Corps involvement in Departmental emergency preparedness and response activities;
- To protect and advance the health of the Nation through educating the public; advocating for effective disease prevention and health promotion programs and activities; and, provide a highly recognized symbol of national commitment to protecting and improving the public's health;
- To articulate scientifically based health policy analysis and advice to the President and the Secretary of Health and Human Services (HHS) on the full range of critical public health, medical, and health system issues facing the Nation;
- To provide leadership in promoting special Departmental health initiatives, e.g., tobacco and HIV prevention efforts, with other governmental and non-governmental entities, both domestically and internationally;
- To elevate the quality of public health practice in the professional disciplines through the advancement of appropriate standards and research priorities; and
- To fulfill statutory and customary Departmental representational functions on a wide variety of Federal boards and governing bodies of non-Federal health organizations, including the Board of Regents of the Uniformed Services University of the Health Sciences, the National Library of Medicine, the Armed Forces Institute of Pathology, the Association of Military Surgeons of the United States, and the American Medical Association.
- carry out activities to encourage individuals to enter the nursing profession, including providing education on the distinct role of nurses in the health professions and examining nursing issues that would increase public safety, such as issues relating to staff levels, working conditions, and patient input;
- carry out activities to encourage nurses to become educators in schools of nursing;
- carry out activities to promote the public health, including encouraging nurses to be volunteers to projects that educate the public on achieving better health; and
- conduct media campaigns and make personal appearances for purposes of paragraphs (1) through (3).
 The Surgeon-General does not go out promoting the role of doctors (or even surgeons). He promotes public health by overseeing the US Public Health Service Commissioned Corps. That team consists of doctors, nurses and other allied health professionals. Is it not enough that nurses are part of a team? If they want to run the team why doesn't a nurse nominate themselves for the office of Surgeon-General? It's pretty clear that you don't even have to be a surgeon.
The Surgeon-General does not go out promoting the role of doctors (or even surgeons). He promotes public health by overseeing the US Public Health Service Commissioned Corps. That team consists of doctors, nurses and other allied health professionals. Is it not enough that nurses are part of a team? If they want to run the team why doesn't a nurse nominate themselves for the office of Surgeon-General? It's pretty clear that you don't even have to be a surgeon.I don't know about you, but I am not in support of this concept. If a nurse wants to come and show that she can lead a team of health professionals then feel free. This is not a bill for a public-health advocate, or even a patient advocate. This is a bill for an Office of the Nurse-Advocate.
Thursday, April 27, 2006
Let's call a spade a spade

What is it with patient records? Why is it that we can never get it right? I have seen patient cards (with the tiny shorthand doctor scrawl trying to make use of every piece of the card before you have to turn it over), envelopes stuffed full of A4 letters folded in half, manilla folders that everything falls out of constantly, all permutations of colour-coding to hasten the onset of psychedelia, and electronic records where you either have to dictate everything, write everything (and then submit it for scanning), or type everything. Even worse, you have to do all three, and then you cross your fingers that the computer system doesn't go down like it did last week.
Hospital paper records have to take the cake, though. I am used to a standard filing system:
- Patient Registration Details
- Outpatient and non-admission ED notes
- Correspondence
- Investigations (Haematology, Biochemistry, Microbiology, Histopathology, Radiology and ECGs at the back)
- Inpatient admissions with one tab per admission (most recent at the front)
- Split admissions into other volumes if necessary
- Volumes split by time period if necessary
- Outpatient Notes (including correspondence)
- Inpatient Notes
- Investigations filed as they occurred during the outpatient or inpatient progress
- No specific operation notes, all op notes written in progress notes
Having a fairly standardised filing system in Australia has its advantages. I know that if I flip to the back of an admission there will always be a sheet of handwritten paper describing each operation done during that admission. If you are a surgical registrar and you do not look at the handwritten notes in a patient's history, you are in for a lot of surprises.
Unfortunately, my pet peeve for the day is the insistence on calling forms by their "MR number". I understand that the Medical Records staff like to identify each form by number so they know where to file them, but does this jargon need to extend to the rest of the hospital?
If you ask me to fill out an "MR24" how the hell do you expect me to know that you mean the drug chart? And how am I meant to know that an "MR21" is a request for OT assessment? Or that "MR15" is a Progress Note? I am much more interested in whether you can accurately fill out a Fluid Balance chart, not an "MR76"!!!
So for the benefit of any professional form designers out there, anybody who asks me to fill out an MR-something will be met with a blank stare, and "What?". I will feign ignorance until I am told what this form actually is and what it is for. As for forms that have 20 tick boxes and 30 items to circle... I circle or tick the minimum number that will get the job done (usually this involves no more than three). If your form involves more than three selections, then you will get a big black texta mark saying "This form is too complicated". And if you don't like it, you can fill out an MR69 and file it in the round filing cabinet on the floor.
Monday, April 17, 2006
Record Surgery Makes Good News?
This was recently in the news.
Let me ask a question - who cares? I feel sorry for the poor administrator / media liaison manager who felt that this was something to be proud of and worthy of generating a press release. Clearly the reporter didn't know what to make of it. Neither do I. Let's just hope that this does not set off a round of "I do more operations that you" comparisons. Before we know it, there will be tearoom arguments at the DHS about it. I'll nominate this week's Bullshit Bingo phrases now:
By the way, is it just me, or does the ABC news just recycle the same operating theatre photo again and again?
Qld hospitals set surgery record
Queensland's two largest hospitals have set records for the amount of surgery they performed last month. More surgical cases were handled at the Princess Alexandra Hospital than at any other time in its history. The Royal Brisbane and Women's Hospital set a March record for the number of surgeries performed this year. Staff at the PA Hospital operated on more than 1,700 patients in March and more than 2,000 patients were treated at the Royal Brisbane.
Let me ask a question - who cares? I feel sorry for the poor administrator / media liaison manager who felt that this was something to be proud of and worthy of generating a press release. Clearly the reporter didn't know what to make of it. Neither do I. Let's just hope that this does not set off a round of "I do more operations that you" comparisons. Before we know it, there will be tearoom arguments at the DHS about it. I'll nominate this week's Bullshit Bingo phrases now:

- statistical anomaly
- population-adjusted operation rate
- minor-major Procedure ratio
- theatre utilisation
- staff efficiency index
By the way, is it just me, or does the ABC news just recycle the same operating theatre photo again and again?
Monday, April 10, 2006
All I need is a knife, spork and foon!
 On a lighter note, one of my colleagues is known for not being fussy with his surgical instruments. As a surgical registrar, often you are subject to the vagaries of available equipment at your hospital. In many cases the instruments you want or prefer may have just been put into the steriliser (and thus unavailable for the next four hours), or in use in another theatre, or not on your scrub nurse's tray, or dropped on the floor, or just plain don't exist.
On a lighter note, one of my colleagues is known for not being fussy with his surgical instruments. As a surgical registrar, often you are subject to the vagaries of available equipment at your hospital. In many cases the instruments you want or prefer may have just been put into the steriliser (and thus unavailable for the next four hours), or in use in another theatre, or not on your scrub nurse's tray, or dropped on the floor, or just plain don't exist.One learns to be versatile, and a pair of forceps becomes a blunt dissection tool, a retractor, and a needle holder. A pair of artery forceps (or, as those surgeons on the other side of the pond call them, "hemostats") becomes a towel clip, a retractor, a blunt dissector, a temporary replacement for dressing tape, and many other uses that only become obvious at the time.
In any case, this colleague was known for saying (when asked, "What instruments will you need?") "A knife, fork and spoon please."
Lo and behold, one day he was handed a sterilised kitchen cutlery set. The nurses were kind enough to open some real surgical instruments after they had finished laughing at their joke.
 Having said that, though, a spoon actually does a pretty good job of removing thrombus from the inside of aortic aneurysms.
Having said that, though, a spoon actually does a pretty good job of removing thrombus from the inside of aortic aneurysms.On the subject of spoons, this article recently came to my attention. I can only say that epidemiologists have a lot of time on their hands.
Sunday, April 02, 2006
We all have to start somewhere!
 I currently have the pleasure of my junior registrar being on leave. This is especially so because she has been replaced by an even more junior registrar. In fact, this registrar is so junior that he doesn't know what being a registrar actually means.
I currently have the pleasure of my junior registrar being on leave. This is especially so because she has been replaced by an even more junior registrar. In fact, this registrar is so junior that he doesn't know what being a registrar actually means.Thankfully for him, I do remember what it was like being a registrar for the first time. It is, in fact, just like every other transition that we make in our personal lives and professional careers... learning to trust your own judgement, realising that other people are not always smarter or more knowledgable than you, and accepting that the greater responsibility that comes with being senior means that you have to always keep in mind the "bigger picture". That means that the patient is not your only responsibility.
Perhaps the biggest lesson of all is that there are times when, if you don't do it, nobody will.
While these may seem like very generic observations, they are nonetheless true. As you progress in seniority, they become more and more evident. Unfortunately, there are many health professions where these tenets do not apply.
NHS Blog Doctor's favourite topic at the moment is Nurse Practitioners. I must admit that I think there are some very good Nurse Practitioners out there. They are the ones who know their limitations, and stick to the very straight and narrow area that they are trained in. Unfortunately there are also many who do not, and think that with their protocols and limited clinical skills they can deal with situations that many doctors take years to start to understand.
As a neurosurgical registrar, I had to learn to confidently assess and clear cervical spines. Nobody was going to do this for me. If I made a mistake I had to wear the blame. Perhaps I left a few collars on for longer than necessary, and ordered a few more flexion-extension views than necessary, but that's what it took until I became comfortable with my clinical acumen and responsibilities.
As a vascular surgery covering registrar, I learnt to keep track of my consultants. They changed their on-call rotations regularly, and I could not trust switchboard to keep track correctly. If a AAA came in I had to know who to call, and where they would be. There was little luxury in delay while I tried five different phone numbers.
As a trauma surgery registrar, I had to learn to deal with team conflict. Consultants did not get along, ward rounds were dysfunctional. Politics were rife. Nevertheless, I did my best to smooth things over and ensure that the unit functioned and served its patients well. Was this part of my job description? No, but who else was there to turn to?
As a general surgery registrar, I learnt to deal with private rooms, secretaries, nagging patients from the waiting list, pre-admission stuff-ups, and a barely competent intern going through a divorce. This wasn't part of my medical school training, but one has to accept that as the interface between almost all parts of the hospital and the community, the registrar becomes the non-stop troubleshooting machine.
There have been many other clinical and non-clinical lessons that I have learnt along the way, and it has taken many years to develop my skills and better judgement. Each rotation through an unrelated field, different hospital, different state and different country has only served to teach me how everything can change around me, and yet I am still expected to (and more importantly, able to) oversee every aspect of my patients' care. I can happily say that I can see how "the system" works (or doesn't work) and appreciate the point of view of most other parties in "the system". That doesn't mean that I agree with them, but I think it makes me a better doctor.
I happily admit that my job does not start at 9am and finish at 5pm. That is the nature of being a doctor - or even worse, a surgeon. My responsibilities stay with me when I go home, they carry on for years. Long after I retire I will still be responsible for everything I have done for my patients. If I did not want this responsibility I would never have progressed beyond being a hospital resident. Hmmm... now that is an interesting idea. Perhaps there is a hidden social agenda - given the current need for hospital resident doctors, by scaring them away from becoming registrars and consultants we can increase the RMO workforce? Another topic for another day, I fear.
Sunday, March 26, 2006
Is "Monopoly" a Tautology?
Recently the Royal Australasian College of Surgeons released a workforce study of current fellows along with a media release on the 21st of March stating:
Really? I would imagine that most 55 year-olds would plan to retire within 15 years, and given that only practising fellows were surveyed the mean age of 55.5 years is probably not unexpected. Neither is the fact that 16 per cent of fellows are under 40. Nevertheless, I can't knock The Russter's activist attitude in righting the public misconceptions of surgical training in Australia. My favourite was this line from the press release:
What math? Sorry, you lost me there, Russ.
Understandably, most media outlets followed this up with fairly predictable reports:
Not to stop there, 2 days later she decided to follow up with an article on Our Mate Vin but instead has muddied the waters further.
What concerns me (as I have said previously) is that I do not know whether reporters like Carol are merely ignorant of the issues truly facing specialist training (and is therefore being manipulated by political interest groups) or whether she is deliberately misrepresenting the situation for the purpose of newspaper sales.
Firstly, the university consortium is interested in expanding into all specialties, so why is the article a focus on "Battle over surgical monopoly"? Because surgeons make more interesting news than, say ... neuropsychiatrists. ("Who are neuropsychiatrists?", you may well ask. They are those doctors who, for example, would be interested in whether depressed people who think about ducks have more sensitive serotonin receptors in their amygdala - now try writing a front page news article about that!)
The other reason is that the ACCC has taken the trouble to investigate the RACS' role in surgical training - which makes you wonder why the ACCC targeted surgeons in the first place. At this point it becomes a revolving argument.
 Secondly, it is correct that Vin Massaro was CEO of the RACS from 1999 to 2003. I am not privy to his reasons for leaving the college or being hired by this university consortium, but it is just plain wrong to refer to him as "Uni push surgeon a college veteran". Our Mate Prof Vin is not a surgeon, or a medical doctor, but an academic with an interest in higher education policy. He worked very hard to represent the college of surgeons' interests when working with them, and now presumably works very hard to represent this consortium's interest (even if to the detriment of the college).
Secondly, it is correct that Vin Massaro was CEO of the RACS from 1999 to 2003. I am not privy to his reasons for leaving the college or being hired by this university consortium, but it is just plain wrong to refer to him as "Uni push surgeon a college veteran". Our Mate Prof Vin is not a surgeon, or a medical doctor, but an academic with an interest in higher education policy. He worked very hard to represent the college of surgeons' interests when working with them, and now presumably works very hard to represent this consortium's interest (even if to the detriment of the college).
Thirdly, Our Mate Vin's submission to the ACCC as reported by Carol suggests that:
Perhaps Our Mate Vin should consider the fact that training systems in the UK are no shorter than in Australia, and that the latest revolution in US surgical traning is to implement schemes remarkably similar to (and almost as long as) those that exist here. And do you seriously believe that shorter and less training will not affect the quality of clinical services among graduates? I guess we can cut the medical course back from six years to four then... oh we have already done that. My bad.
At best I can only assume that the Vinster is not talking about shortening surgical training, but skipping internship and junior HMO jobs, where we learn the essentials of being a real-world doctor. Where we learn to respect the methods of our colleagues in other specialties, so that we can see the bigger picture when treating our patients. Where we can see and then decide which specialty we would actually consider working in. Where we act as the backbone of the public hospital system by doing all the day-to-day work like putting in IVs, writing drug charts, ordering and checking pathology and radiology tests, talking to patients and staying up all night to deal with those 3am acute febrile / hypertensive / nausea / insomnia / psychotic episodes. Yes, let's get rid of those doctors so that we can yo-yo the number of trainees in the pipeline temporarily.
But it does not take a rocket scientist to see that if I have to do 100 supervised rhubarbectomies to qualify as a rhubarb surgeon, and I only see 20 cases a year, then it will take... oh let's see, 5 years. So if we introduce an "alternative pathway" then my mate and I have to share the rhubarbs, and get 10 each a year... hang on, now I have to train for 10 years! How does that generate surgeons any faster? Oh, I see, we will just go to lectures on rhubarb theory and practise on rubber rhubarbs instead.
Fourthly, Old Vinnie Boy knows full well that the current rate-limiting step in the production of qualified, competent specialist surgeons is the provision of accredited training posts by the State and Federal Governments. He has said so himself. The State Governments have an interest in preventing basic surgical trainees from entering specialty training - that way they generate a glut of hospital medical officers, driving down salaries and conditions so that these doctors can have the privilege of being overworked and underpaid to give their all caring for patients. The Federal Government has an interest in limiting specialist numbers because this prevents patients having more access to surgery, procedures and drugs, all of which they would have to fund.
Perhaps Our Mate Vin knows more than he is letting on... is setting up an "alternative pathway" code for "time to pay up, Governments"? The universities can only fund training if they start paying the trainers, something that the RACS has enough loyalty among fellows to avoid currently. All of that goodwill may evaporate soon if the current push to commodify surgical training continues. And given that accredited training jobs will not increase unless funding increases, any agreement by the Governments to fund university teaching will probably lead to a widespread funding increase to all parties (RACS, Hospitals and Universities). Somehow I think that ain't gonna happen.
Sadly, it is public perception (and that of the ACCC) that surgeons have a vested interest in limiting their own numbers. If that were so, we would not be giving up our time and energy pro bono (according to Russ-boy, $240 million worth a year) to train our colleagues, we would not be asking Government to fund more training positions, and we would be looking forward to our workload increasing, year by year, until we all died of exhaustion.
Perhaps it is against the tidal wave of public opinion, but I believe that surgeons, like all other doctors, have the primary goal of giving our patients the best possible care that we can provide.

"Nearly 50 per cent of the Australian surgical workforce is over 55 and is set to retire within the next 15 years, just as we start to experience the biggest ever demand for surgical services."
Really? I would imagine that most 55 year-olds would plan to retire within 15 years, and given that only practising fellows were surveyed the mean age of 55.5 years is probably not unexpected. Neither is the fact that 16 per cent of fellows are under 40. Nevertheless, I can't knock The Russter's activist attitude in righting the public misconceptions of surgical training in Australia. My favourite was this line from the press release:
"It takes 10 years to train a surgeon. You do the maths - we are running out of time."
What math? Sorry, you lost me there, Russ.
Understandably, most media outlets followed this up with fairly predictable reports:
- Doctors Warn of Surgeon Shortage, ABC 22/3/06
- Dad's army: half of all surgeons want to retire within 15 years, Sydney Morning Herald 22/3/06
- Where have all the surgeons gone?, NineMSN / Nine News 21/3/06
- Ageing crisis in surgery, Herald Sun 22/3/06
- Surgeon shortage crisis on horizon, The Advertiser 22/3/06
Not to stop there, 2 days later she decided to follow up with an article on Our Mate Vin but instead has muddied the waters further.
What concerns me (as I have said previously) is that I do not know whether reporters like Carol are merely ignorant of the issues truly facing specialist training (and is therefore being manipulated by political interest groups) or whether she is deliberately misrepresenting the situation for the purpose of newspaper sales.
Firstly, the university consortium is interested in expanding into all specialties, so why is the article a focus on "Battle over surgical monopoly"? Because surgeons make more interesting news than, say ... neuropsychiatrists. ("Who are neuropsychiatrists?", you may well ask. They are those doctors who, for example, would be interested in whether depressed people who think about ducks have more sensitive serotonin receptors in their amygdala - now try writing a front page news article about that!)
The other reason is that the ACCC has taken the trouble to investigate the RACS' role in surgical training - which makes you wonder why the ACCC targeted surgeons in the first place. At this point it becomes a revolving argument.
 Secondly, it is correct that Vin Massaro was CEO of the RACS from 1999 to 2003. I am not privy to his reasons for leaving the college or being hired by this university consortium, but it is just plain wrong to refer to him as "Uni push surgeon a college veteran". Our Mate Prof Vin is not a surgeon, or a medical doctor, but an academic with an interest in higher education policy. He worked very hard to represent the college of surgeons' interests when working with them, and now presumably works very hard to represent this consortium's interest (even if to the detriment of the college).
Secondly, it is correct that Vin Massaro was CEO of the RACS from 1999 to 2003. I am not privy to his reasons for leaving the college or being hired by this university consortium, but it is just plain wrong to refer to him as "Uni push surgeon a college veteran". Our Mate Prof Vin is not a surgeon, or a medical doctor, but an academic with an interest in higher education policy. He worked very hard to represent the college of surgeons' interests when working with them, and now presumably works very hard to represent this consortium's interest (even if to the detriment of the college).Thirdly, Our Mate Vin's submission to the ACCC as reported by Carol suggests that:
"The Commission should reconsider the involvement of medical schools in the training of specialists, through a parallel stream of training, so that new training pathways can be tested. These could include enabling students to begin their specialisation studies while undertaking their initial qualification thus reducing the length of the specialist training programs. Reducing the length of the training program would not directly affect the standard of clinical services or the quality of the graduates. Australia has a longer training program than the US and Canada (and now the UK), yet the standard of health care in those countries cannot be regarded as inferior to Australia's."
Perhaps Our Mate Vin should consider the fact that training systems in the UK are no shorter than in Australia, and that the latest revolution in US surgical traning is to implement schemes remarkably similar to (and almost as long as) those that exist here. And do you seriously believe that shorter and less training will not affect the quality of clinical services among graduates? I guess we can cut the medical course back from six years to four then... oh we have already done that. My bad.
At best I can only assume that the Vinster is not talking about shortening surgical training, but skipping internship and junior HMO jobs, where we learn the essentials of being a real-world doctor. Where we learn to respect the methods of our colleagues in other specialties, so that we can see the bigger picture when treating our patients. Where we can see and then decide which specialty we would actually consider working in. Where we act as the backbone of the public hospital system by doing all the day-to-day work like putting in IVs, writing drug charts, ordering and checking pathology and radiology tests, talking to patients and staying up all night to deal with those 3am acute febrile / hypertensive / nausea / insomnia / psychotic episodes. Yes, let's get rid of those doctors so that we can yo-yo the number of trainees in the pipeline temporarily.
But it does not take a rocket scientist to see that if I have to do 100 supervised rhubarbectomies to qualify as a rhubarb surgeon, and I only see 20 cases a year, then it will take... oh let's see, 5 years. So if we introduce an "alternative pathway" then my mate and I have to share the rhubarbs, and get 10 each a year... hang on, now I have to train for 10 years! How does that generate surgeons any faster? Oh, I see, we will just go to lectures on rhubarb theory and practise on rubber rhubarbs instead.
Fourthly, Old Vinnie Boy knows full well that the current rate-limiting step in the production of qualified, competent specialist surgeons is the provision of accredited training posts by the State and Federal Governments. He has said so himself. The State Governments have an interest in preventing basic surgical trainees from entering specialty training - that way they generate a glut of hospital medical officers, driving down salaries and conditions so that these doctors can have the privilege of being overworked and underpaid to give their all caring for patients. The Federal Government has an interest in limiting specialist numbers because this prevents patients having more access to surgery, procedures and drugs, all of which they would have to fund.
In a letter to federal Health Minister Tony Abbott this month, the universities said they hoped to start providing post-graduate specialist training as early as 2007. They will seek approval from the Australian Medical Council, which provides accreditation for training. They have also asked governments to fund training places in hospitals.
...
College of Surgeons president Russell Stitz said the college would be "quite happy" to work in partnership with universities, but said it would be unrealistic for them to become alternative providers at the moment. "They haven't got the capacity, they don't have surgeons that they can draw on, and how are they going to do it? Are they going to pay the surgeons? Because I can tell you the surgeons are not going to work for the universities for nothing."
Perhaps Our Mate Vin knows more than he is letting on... is setting up an "alternative pathway" code for "time to pay up, Governments"? The universities can only fund training if they start paying the trainers, something that the RACS has enough loyalty among fellows to avoid currently. All of that goodwill may evaporate soon if the current push to commodify surgical training continues. And given that accredited training jobs will not increase unless funding increases, any agreement by the Governments to fund university teaching will probably lead to a widespread funding increase to all parties (RACS, Hospitals and Universities). Somehow I think that ain't gonna happen.
Sadly, it is public perception (and that of the ACCC) that surgeons have a vested interest in limiting their own numbers. If that were so, we would not be giving up our time and energy pro bono (according to Russ-boy, $240 million worth a year) to train our colleagues, we would not be asking Government to fund more training positions, and we would be looking forward to our workload increasing, year by year, until we all died of exhaustion.
Perhaps it is against the tidal wave of public opinion, but I believe that surgeons, like all other doctors, have the primary goal of giving our patients the best possible care that we can provide.

Saturday, March 18, 2006
Needlesticks and Surgery
 Barbados Butterfly recently posted about her needlestick injury. I hope she is feeling better. I have had three official "patient body fluid exposure incidents" during my career. They were:
Barbados Butterfly recently posted about her needlestick injury. I hope she is feeling better. I have had three official "patient body fluid exposure incidents" during my career. They were:- Giving mouth to mouth at a roadside accident as a medical student, unfortunately to a fatally injured Hep-C positive patient
- With a solid round-bodied needle during a difficult low anterior resection (no stapler)
- At the end of last year, topping up a wound with local anaesthetic at the end of the case.
 By far and away, though, I think the biggest contribution to avoiding needlestick injuries are the needleless infusion systems, using IV bungs (reflux valves) and Luer locks. Unfortunately many hospitals are too cheap to stock true Luer lock syringes (that twist and lock in) and just get Luer slip syringes. In that setting spray exposure from a loose fitting syringe-to-bung is rather common.
By far and away, though, I think the biggest contribution to avoiding needlestick injuries are the needleless infusion systems, using IV bungs (reflux valves) and Luer locks. Unfortunately many hospitals are too cheap to stock true Luer lock syringes (that twist and lock in) and just get Luer slip syringes. In that setting spray exposure from a loose fitting syringe-to-bung is rather common.The needle and the blade will not disappear in the foreseeable future of open surgery. Needlesticks are and will still be a fact of life. I was recently offered specific "needlestick infection insurance", and on reading through the paperwork, the payout was a lump sum on confirmation of new-onset infection:
"A benefit will not be payable if: ... a medical cure is found for Acquired Immune Deficiency Syndrome (AIDS), or the effects of the HIV virus, Hepatitis B or Hepatitis C, or in the event of a treatment being developed and approved which makes these viruses inactive and non-infectious."Even if such treatment is hideously expensive or years away from market availability?
"... you have AIDS or any AIDS related disorder or a positive blood test... unless you are able to provide evidence, in the form of sequence analysis of the source and index virus strains, satisfactory to us that the accident involved the definitive source of the virus."
Why would I be applying for this cover if I already had HIV? What kind of product do these guys think they are offering? I think I will rely on my Income Protection Insurance, so I have thrown it in the bin.
Monday, March 13, 2006
Doctors get stressed too!
 In light of recent events, I must point out to all doctors (and other medical professionals) that stress is a daily part of our work, and that there are things that can be done about it.
In light of recent events, I must point out to all doctors (and other medical professionals) that stress is a daily part of our work, and that there are things that can be done about it.Unfortunately we work in a profession that is gradually being broken up into little pieces. Doctors used to do everything, make diagnoses, do the laboratory tests, check our own histology, grind up our medicines, dress all the wounds, counsel the patients, and lead them through their exercise and rehabilitation program. Nurses have always been our partners in most of this care.
Increasingly, much of our work is now delegated, either to other specialist colleagues (pathology, radiology) or to other, newer, allied health groups such as physiotherapists, psychologists, radiographers, occupational therapy, dietetics, anaesthetic technicians, phlebotomists, ECG technicians. While their roles are quite clearcut, the doctor's role is no longer. Like ward nurses, we have to pick up, sort out, and deal with any problems or issues that falls into the cracks between these other groups. We become a hospital "dumping ground" because if something is nobody else's fault or problem, it is still ours when we come back to work the next day. Even worse, we bear the brunt of the social and medicolegal responsibility of all of this work, and that responsibility does not stop at 5.30pm on weekdays.
On top of all of that, we deal with the whole spectrum of human emotions with our patients, and then we are expected to go home and balance our personal lives in the midst of overwhelming work and study requirements. It is not surprising that the incidence of "burnout", "nervous breakdowns" and suicides among doctors is among the highest of all professions. Interestingly, attempted suicides are rare among doctors... knowledge and access means that they almost always succeed.
 So if you feel that you or a colleague are over-stressed, not coping, depressed, overwhelmed, or unsafe, then take a step back. Take a deep breath, look objectively at what damage you are doing to yourself, your patients, and your family. If the problem is not one you can solve alone, then turn to someone who can help, whether it be your professional association, a friend, or an organisation like the VDHP.
So if you feel that you or a colleague are over-stressed, not coping, depressed, overwhelmed, or unsafe, then take a step back. Take a deep breath, look objectively at what damage you are doing to yourself, your patients, and your family. If the problem is not one you can solve alone, then turn to someone who can help, whether it be your professional association, a friend, or an organisation like the VDHP.
Saturday, March 11, 2006
At least it wasn't a person!
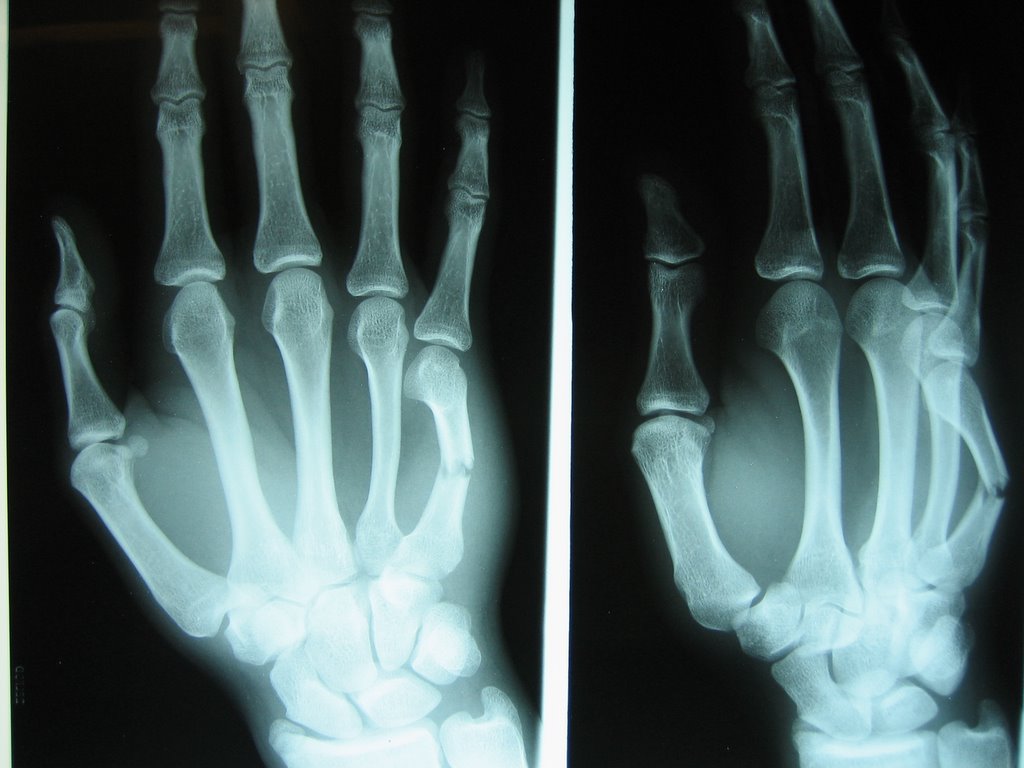
Gasbagging recently put up some photos of a 5th Metacarpal shaft fracture (not quite technically a Boxer's Fracture).
It always amazes me that often these patients present with a typical story:
"I was ropeable. I was pumped up and about to hit someone... so at least I punched a wall (or a window) and not a person!"
What is it about them that they think they have to punch something? Why can't they contain their rage or vent it elsewhere (onto something soft)? As far as I can tell, there is about as much justification for punching a wall as self-mutilation. Oh, perhaps that is a topic for some other day.
Saturday, February 18, 2006
RU486? IM4 Due Process
1996 - Senator Brian Harradine successfully introduces the Therapeutic Goods Amendment Bill 1996 to limit the introduction of pharmacological abortifacients (drugs intended to induce abortion) by taking away the Therapeutic Goods Administration's (TGA's) ability to assess any such drugs unless prior approval is given by the Minister for Health and Ageing. All such drugs are classified under the name of "Restricted Goods".
The intention was to introduce an added layer of Governmental scrutiny to any attempts to widen the options for women seeking abortion, and presumably to deter any health providers from offering pharmacological abortion (a de facto ban).
Since that time, no pharmaceutical company has made any attempts to apply to import or supply RU486 (Mifepristone) for pharmacological abortion in Australia, most likely on the belief that all presiding Health Ministers would have declined to permit the application from proceeding.
October 2005 - Debate develops over Health Minister Tony Abbott's public anti-abortion stance, and the Democrats state their intention to repeal Tony Abbott's right to veto any application to introduce pharmacological abortifacients (in particular RU486).
November 2005 - Tony Abbott clearly states his opposition to the use of RU486 on the basis of a report from the Chief Medical Officer Professor Andrew Child which is widely criticised.
29 November 2005 - Thoughful Parliamentary Library article on current status of RU486 in Australia.
December 2005 - Professor Caroline de Costa makes the first application to the TGA for a license to prescribe RU486 as a test case.
8 December 2005 - This application prompts Senators Nash, Troeth, Allison and Moore seek to introduce the Therapeutic Goods Amendment (Repeal of Ministerial Responsibility for Approval of RU486) Bill 2005. Background report here.
8 January 2006 - Several more Obstetricians state their intention to apply for a license to prescribe Mifeprostone.
13 February 2006 - The Bill is debated and passed in the Senate.
16 February 2006 - The Bill is debated and passed in the House of Parliament despite attempts to confuse the voting process with multiple amendments.
On Due Process
The TGA has the power as an independent statutory authority to assess all medicines, pharmaceuticals, and therapeutic devices. The items it assesses are not always used only for therapeutic purposes, and often they are used in combination with other procedures or medicines. It has an expert, world-recognised panel to do these assessments, and we entrust them on a day-to-day basis to assess and approve (or decline) all medicines and medical instruments that are in current use.
So why did Senator Harradine wish to remove the authority to review abortifacients from the TGA? This has nothing to do with the TGA's ability or suitability to objectively assess this class of drugs, but merely with his own personal viewpoints that abortion is not acceptable, and any means of preventing access to abortion should be implemented. Therefore a class of "restricted goods" was created which was intended purely to stop one drug entering the country for one specific purpose. This creates an administrative and logical divide - that surgical abortion is allowed but pharmacological abortion is not. This has nothing to do with safety, but was merely Senator Harradine's first step towards banning abortion altogether.
It was about time that commonsense prevailed, and the TGA was allowed to go back to doing its job - assessing the risks and benefits of all therapeutic agents presented to it and making sure that they are used safely and appropriately without the interference of the Parliament.
If the Government wishes to outlaw abortion, then introduce a law to outlaw abortion, do not undermine the currently effective system for assessment and regulation of therapeutic agents by adding beauracratic red tape.
There is a reason why the TGA is empowered to review these agents - because they are experts and they review medical and scientific evidence critically. Based on the tragic misuse of statistics, omission and manipulation of facts, pseudofacts, and illogical arguments during the course of the recent debate in the House of Parliament, it is self-evident why politicians and the Parliament is not entrusted with the critical evaluation of drugs and medicines.
On Abortion
There is no doubt that the whole issue about access to abortion facilities (including counselling services) is one that generates major angst amongst parts of the community. Any event that leads to a perception of loss is traumatic and distressing. As doctors we deal with this every day, patients get upset when their body changes, either because of their own pathology or disease, or because of what is done to them.
The loss of a foetus is even more distressing for any woman because not only is there a perception that their own body is affected, but a potential life. I deliberately use the word "potential" because there is no way to know, either as a layperson, a scientist or any other professional, at what stage a life is involved. What matters most is how the patient or mother regards that potential life, and what attachment she holds to it, and the consequences of allowing that potential life to develop (or not develop, as the case may be). It is her body, and she is the major stakeholder.
Just as the public have no right to tie her down and make her abort or miscarriage, the public have no right to tie her down and stop her from aborting or miscarrying. It is not practicable to deny this choice to women, so the goal of facilitating abortion is one of harm minimisation. Those who reject a woman's right to supervised abortion services must in principle also reject anti-smoking advertisements.
At the Coalface
A purely hypothetical young lady in her early 20s presented to a country hospital with severe right iliac fossa pain (right lower abdomen) for several days. She was also 12 weeks pregnant, which was not wanted. Her obstetrician was a devout Catholic who had declined to perform a suction termination of pregnancy on religious grounds, and no other obstetrician was available to treat her. When it became clear that this young girl had appendicitis she declined surgery, hoping that this would lead to a spontaneous abortion. After 2 days she got what she wanted, at the cost of a perforated appendix and a big scar down the middle of her belly.
"restricted goods means medicines (including progesterone antagonists and vaccines against human chorionic gonadotrophin) intended for use in women as abortifacients.
— Therapeutic Goods Amendment Bill 1996
The intention was to introduce an added layer of Governmental scrutiny to any attempts to widen the options for women seeking abortion, and presumably to deter any health providers from offering pharmacological abortion (a de facto ban).
Since that time, no pharmaceutical company has made any attempts to apply to import or supply RU486 (Mifepristone) for pharmacological abortion in Australia, most likely on the belief that all presiding Health Ministers would have declined to permit the application from proceeding.
October 2005 - Debate develops over Health Minister Tony Abbott's public anti-abortion stance, and the Democrats state their intention to repeal Tony Abbott's right to veto any application to introduce pharmacological abortifacients (in particular RU486).
November 2005 - Tony Abbott clearly states his opposition to the use of RU486 on the basis of a report from the Chief Medical Officer Professor Andrew Child which is widely criticised.
29 November 2005 - Thoughful Parliamentary Library article on current status of RU486 in Australia.
December 2005 - Professor Caroline de Costa makes the first application to the TGA for a license to prescribe RU486 as a test case.
8 December 2005 - This application prompts Senators Nash, Troeth, Allison and Moore seek to introduce the Therapeutic Goods Amendment (Repeal of Ministerial Responsibility for Approval of RU486) Bill 2005. Background report here.
8 January 2006 - Several more Obstetricians state their intention to apply for a license to prescribe Mifeprostone.
13 February 2006 - The Bill is debated and passed in the Senate.
16 February 2006 - The Bill is debated and passed in the House of Parliament despite attempts to confuse the voting process with multiple amendments.
On Due Process
The TGA has the power as an independent statutory authority to assess all medicines, pharmaceuticals, and therapeutic devices. The items it assesses are not always used only for therapeutic purposes, and often they are used in combination with other procedures or medicines. It has an expert, world-recognised panel to do these assessments, and we entrust them on a day-to-day basis to assess and approve (or decline) all medicines and medical instruments that are in current use.
So why did Senator Harradine wish to remove the authority to review abortifacients from the TGA? This has nothing to do with the TGA's ability or suitability to objectively assess this class of drugs, but merely with his own personal viewpoints that abortion is not acceptable, and any means of preventing access to abortion should be implemented. Therefore a class of "restricted goods" was created which was intended purely to stop one drug entering the country for one specific purpose. This creates an administrative and logical divide - that surgical abortion is allowed but pharmacological abortion is not. This has nothing to do with safety, but was merely Senator Harradine's first step towards banning abortion altogether.
It was about time that commonsense prevailed, and the TGA was allowed to go back to doing its job - assessing the risks and benefits of all therapeutic agents presented to it and making sure that they are used safely and appropriately without the interference of the Parliament.
If the Government wishes to outlaw abortion, then introduce a law to outlaw abortion, do not undermine the currently effective system for assessment and regulation of therapeutic agents by adding beauracratic red tape.
There is a reason why the TGA is empowered to review these agents - because they are experts and they review medical and scientific evidence critically. Based on the tragic misuse of statistics, omission and manipulation of facts, pseudofacts, and illogical arguments during the course of the recent debate in the House of Parliament, it is self-evident why politicians and the Parliament is not entrusted with the critical evaluation of drugs and medicines.
On Abortion
There is no doubt that the whole issue about access to abortion facilities (including counselling services) is one that generates major angst amongst parts of the community. Any event that leads to a perception of loss is traumatic and distressing. As doctors we deal with this every day, patients get upset when their body changes, either because of their own pathology or disease, or because of what is done to them.
The loss of a foetus is even more distressing for any woman because not only is there a perception that their own body is affected, but a potential life. I deliberately use the word "potential" because there is no way to know, either as a layperson, a scientist or any other professional, at what stage a life is involved. What matters most is how the patient or mother regards that potential life, and what attachment she holds to it, and the consequences of allowing that potential life to develop (or not develop, as the case may be). It is her body, and she is the major stakeholder.
Just as the public have no right to tie her down and make her abort or miscarriage, the public have no right to tie her down and stop her from aborting or miscarrying. It is not practicable to deny this choice to women, so the goal of facilitating abortion is one of harm minimisation. Those who reject a woman's right to supervised abortion services must in principle also reject anti-smoking advertisements.
At the Coalface
A purely hypothetical young lady in her early 20s presented to a country hospital with severe right iliac fossa pain (right lower abdomen) for several days. She was also 12 weeks pregnant, which was not wanted. Her obstetrician was a devout Catholic who had declined to perform a suction termination of pregnancy on religious grounds, and no other obstetrician was available to treat her. When it became clear that this young girl had appendicitis she declined surgery, hoping that this would lead to a spontaneous abortion. After 2 days she got what she wanted, at the cost of a perforated appendix and a big scar down the middle of her belly.
Monday, February 13, 2006
COAG: Clueless Organisation of Anacoluthic Gits
 Last week I was driving home when I heard the ABC's PM show (yes, I am one of those pompous ABC listeners) summing up the recent COAG meeting.
Last week I was driving home when I heard the ABC's PM show (yes, I am one of those pompous ABC listeners) summing up the recent COAG meeting.While the news about investing in preventative health, mental illness (not that anyone has specified what changes will actually happen - will there be more acute care beds, institutional beds, community housing, CATT teams, or just bureacracy?) is essentially just feel-good news for the benefit of the media, what blew me away was firstly the ongoing failure of the Federal and State Governments to understand the workforce bottlenecks in medical training, and secondly, Peter Beattie's inane suggestions to reform the health system.
In regard to the Australian "doctor-shortage" - the Howard Goverment fails to realise that this is a problem on multiple levels created by its own attempt to reign in Medicare. On defeating the Keating Goverment in 1996 one of the early acts of the Howard Government was to restrict the availability of Provider Numbers. These numbers are how GPs and specialists are paid by Medicare every time they see a patient. The goal of this was obvious - fewer doctors who can claim money from the public purse means paying out less money, and encouraging competition for scarce funds. It also meant that the Federal Government could then place restrictions on what doctors had to do to earn the right to a Provider Number (e.g. work in the country, complete a specialist or Family Medicine training program). Many organisations spoke out against these changes, and doctors went on rallies and strikes to oppose it.
Doctors who were graduating from medical school found that they could no longer work as GPs, so what happened? They either did what the Government wanted and stuck around for training, or headed off overseas ( the so-called "brain drain" - which actually works both ways). Within a few years, the number of GPs who were able to get Provider Numbers (and thereby work in the public sector) was choked and limited by the State and Federal Government's willingness or otherwise to fund Family Medicine Training positions. Now we see the Howard Government complaining about GPs charging above the (meagre) Medicare Schedule Fees - all because there is now more demand than supply and John Howard's competitive marketplace is coming to fruition. Mind you, this is happening not only in GP-land, but in every specialty of modern medicine.
So what does COAG do? It announces that (from PM) "While for now the Federal Government won't lift the number of medical students it funds to go to university, there will be more room for full-fee paying students." Well, DUH! The Federal Government didn't need to do that... Universities could have done that all on their own. All that means is that: 1. More overseas students can come and train in our universities and hospitals so that they can then go back to where they came from and Australia gains no benefit (besides pocketing their money); and 2. More doctors will graduate and increase the backlog of doctors that can't work in the community.
Yes, you read me correctly, doctors that can't work. The people that are rubbing their hands with glee are the hospital administrators who are seeing the number of hospital resident and registrar applications increase, but only small increases in the number of registrars completing their training and becoming Specialists who can go out and serve the Australian community.
The stranglehold on Specialist Training rests with the State Governments (and in the case of GPs, the Federal Government). Specialist colleges like the Royal Australasian College of Surgeons, Royal Australasian College of Physicians, and Royal Australian College of General Practitioners merely accredit jobs as being suitable for training, and administer the courses and examinations to ensure that graduating specialists are up to scratch.
For surgeons and physicians, these are hospital posts that are funded by the State Government via each Hospital's budget, and are decided between each State Governement and Hospital. For GPs, these are via the allocation of restricted Provider Numbers by the Health Insurance Commission (and therefore, Federal Government).
So for the State and Federal Government to blame the Colleges for restricting specialist numbers is farcical. There are literally hundreds if not thousands of hospital doctors half-way through their training, waiting for a funded position to become available so that they can complete their training. Perhaps 1 in 3 of these applicants will get a position each year. The rest either become disenchanted and drop out of medicine (there are plenty of companies looking for such bright-minded people), head overseas, or fill in as locum doctors for all the gaps in the public health system. Even worse, there are those who have completed their specialist training but cannot find a hospital with enough money to employ them... so they head overseas!
At least Peter Beattie understands this part of the equation when he commented:
"…that we've got to stop thinking just about public hospitals being the provider of clinical training. The proposal that I've talked about and which I put to COAG today involves, in Queensland at least, Greenslopes Private Hospital will actually provide that training. Now, yes, there will be some follow-up that'll have to be done by the public hospital system, but we've got to stop thinking about training just being in the public system. We can do this in partnership with the private system. The whole area of health is public/private anyway, here you've got a hospital that will 60 doctors, hopefully starting – up to 60 doctors – hopefully starting this year."
Note that he actually means 60 full-fee paying medical student places, not doctors. But then, why would we quibble over that when what he is actually doing is single-handedly re-defining the whole paradigm of public/private medicine in Australia.
There are a number of reasons why doctors are not routinely rotated to private hospitals for training.
- Patients in a private hospital expect to be treated by their chosen doctor or specialist, not a junior doctor whom the specialist has no choice in and is only doing a 3 month rotation.
- Quality resident medical officers are paid handsomely by private hospitals because they are hand-picked and vetted to do a good job. This new arrangement is a cynical exercise at either cost-cutting at private hospitals (since these training-in-private doctors would presumably be paid at award rates only) and/or reduction in the quality of patient care for the sake of a 30 second soundbite.
- In those rare private hospitals where private surgical registrars have rotated as part of their training program (yes, they already exist), they have no input into the patient's care, and only assist during operations, without performing the crucial parts of the surgery that are the core goal of their training. This is great for the patient, but not good for the trainee.
When doctors are appreciated and rewarded for their work, and allowed to go about their jobs without being pressured left right and centre, they will come back to the public health system. Otherwise, strap yourselves down and get ready for a ride into privatised US-style health care!
Sunday, February 12, 2006
Welcome to The Paper Mask.
I always wondered why people write blogs - why would you go to the trouble of telling the world about all of your mundane little trivialities? Does anybody care? My personal opinion is that it is merely a way to say all of those things that the normal inhibitions of daily life prevent you from doing because you don't want to take responsibility of what comes out of your mouth. You know, all those day-to-day comments like: Did you fart? Those breasts must be fake. George Bush seems like a nice guy. (You get the drift.)
Anyway, I think that the Blog or Weblog must be a way to establish an identity purely on what you say on the blog, not where you live, what you do, what you look like. And if you are embarrassed by what you have said, you just close up shop and move to a new blog. Not, of course, that I am intending to do that.
So what do I have to blog about? Well, not much at the moment, but I am sure that it will come to me. It's inevitable that little details will leak out about who I am or what I do, but there is no need to hurry any of that along.
 On the subject of Paper Masks, however, I did notice something rather odd the other day. One of the hospitals I work at uses Kimberly Clark face masks in the operating theatre. My personal preference is the orange ones, and I hate it when they only come with the big clear plastic shield - I have to carefully rip it off without damaging the rest. So as I was scrubbing, I noticed that the boxes come with this notice on them: “The COLOR ORANGE is a Registered Trademark of Kimberly-Clark Worldwide”.
On the subject of Paper Masks, however, I did notice something rather odd the other day. One of the hospitals I work at uses Kimberly Clark face masks in the operating theatre. My personal preference is the orange ones, and I hate it when they only come with the big clear plastic shield - I have to carefully rip it off without damaging the rest. So as I was scrubbing, I noticed that the boxes come with this notice on them: “The COLOR ORANGE is a Registered Trademark of Kimberly-Clark Worldwide”.
 Now perhaps I'm alone on this one, but I find it rather odd that a company can trademark a colour, or even the phrase “COLOR ORANGE”. Does this mean I now have to pay fees to KC because I've put it up 3 times on a blog? How bizarre!
Now perhaps I'm alone on this one, but I find it rather odd that a company can trademark a colour, or even the phrase “COLOR ORANGE”. Does this mean I now have to pay fees to KC because I've put it up 3 times on a blog? How bizarre!
Anyway, I think that the Blog or Weblog must be a way to establish an identity purely on what you say on the blog, not where you live, what you do, what you look like. And if you are embarrassed by what you have said, you just close up shop and move to a new blog. Not, of course, that I am intending to do that.
So what do I have to blog about? Well, not much at the moment, but I am sure that it will come to me. It's inevitable that little details will leak out about who I am or what I do, but there is no need to hurry any of that along.
 On the subject of Paper Masks, however, I did notice something rather odd the other day. One of the hospitals I work at uses Kimberly Clark face masks in the operating theatre. My personal preference is the orange ones, and I hate it when they only come with the big clear plastic shield - I have to carefully rip it off without damaging the rest. So as I was scrubbing, I noticed that the boxes come with this notice on them: “The COLOR ORANGE is a Registered Trademark of Kimberly-Clark Worldwide”.
On the subject of Paper Masks, however, I did notice something rather odd the other day. One of the hospitals I work at uses Kimberly Clark face masks in the operating theatre. My personal preference is the orange ones, and I hate it when they only come with the big clear plastic shield - I have to carefully rip it off without damaging the rest. So as I was scrubbing, I noticed that the boxes come with this notice on them: “The COLOR ORANGE is a Registered Trademark of Kimberly-Clark Worldwide”. Now perhaps I'm alone on this one, but I find it rather odd that a company can trademark a colour, or even the phrase “COLOR ORANGE”. Does this mean I now have to pay fees to KC because I've put it up 3 times on a blog? How bizarre!
Now perhaps I'm alone on this one, but I find it rather odd that a company can trademark a colour, or even the phrase “COLOR ORANGE”. Does this mean I now have to pay fees to KC because I've put it up 3 times on a blog? How bizarre!Technorati Tags: introduction, paper masks
Subscribe to:
Comments (Atom)






