
When I used to catch the tube in London there was routinely an announcement as the train approached - "Mind the gap please". I am thinking of putting one of these signs up at the private hospital around the corner.
It is not that I have any objection to gap fees - I have some understanding of why they exist. Unfortunately, very little of the general population does. So here comes a brief lesson on the private health insurance system as it stands in Australia. This is part 1 of a 6 part series providing a brief overview of the funding aspects of Health Care in Australia from the perspective of a health professional. I am not an expert in these matters, but hopefully enough to explain how the system works from a practical perspective.
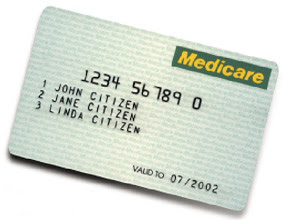
1. Medicare
Medicare is a form of social service support introduced initially in 1975 whereby taxpayer funds cover the basic costs of patients to see doctors in hospitals, clinics, rooms or offices, and even home visits or tele-consulting. More information on the history and development of Medicare is available here and here. The amount of money that the GP or Specialist receives from Medicare is determined by
- How complex the problem is;
- What procedures or services the doctor performs or provides during that consultation;
- How long the doctor spends with the patient or on the consultation.
The original intention was for patients to pay at least a $20 gap fee for any services provided by a doctor (primarily outpatient consultations including seeing, examining, diagnosing, ordering tests, and dispensing treatment to a patient). This evolved to a situation where doctors were given a recommended (CMBS) fee to charge the patient. The patient would then pay the doctor directly and then they would take their bill to a Medicare Office where they would be reimbursed for 75% of the CMBS Fee, effectively leaving the patient out of pocket 25% (the gap fee). Alternatively the patient could take a doctor's invoice to a Medicare Office where they could obtain a cheque written out to the doctor for 75% of the CMBS fee and then pay the remainder to the doctor directly. Cheque fraud by patients was common.
Because there was no cap on a doctor's total fee, the back-and-forth travelling incurred by the patient, and also the fraud problems caused by the above arrangement, the Government then tried to simplify arrangements by introducing Bulk-Billing, which involves doctors undertaking not to charge a gap fee in return to being directly paid 85% of the CMBS fee.
Similar fees apply if a doctor visits a patient at home, or while they are an inpatient in a hospital.
The biggest success of Medicare has been to introduce bulk-billing, and therefore hide the true cost of health care from the patient, effectively saying that health care is free, when the Federal Government is really just buying health care in bulk for its taxpayers, and demanding a discount from doctors while doing so.
In the meantime, the Government uses Medicare to control and dictate who, where, and how doctors practise medicine, by limiting provider numbers (numbers issued to health professionals in order to access Medicare Benefits), bonding doctors to rural placements in order to access benefits, requiring GPs to be "Vocationally Registered" in order to access higher benefits, and placing very specific limitations and conditions on individual procedures and items before claims for benefits can be made. For better or worse, in effect the Federal Government works as a very large US-style Health Maintenance Organisation (HMO).
- Regional doctors back opposition to bonded plan
- ABC Guide to Private Health Insurance
- More incentives urged for rural doctors
- Program aims to encourage country practice
- Islanders turn to witch doctor amid GP crisis
More on this series next week.





No comments:
Post a Comment